Why a physician’s statement is vital to a disability determination
The attending physician’s opinion of their patient’s functional capacity can be one of the most critical elements of any disability review. The attending physician’s statement (APS) is used to help establish the claimant’s functional capacity, among other methods, which is a key factor in determining if an individual is disabled under the terms of their disability insurance policy.
Ideally, this form is completed thoroughly, containing extensive information about medical history, the progression of the individual’s disability condition(s), and the individual’s current functional capacity. Further, the APS can serve in providing information when there are gaps in the medical records, which can be especially important during a pandemic, when medical records may be limited.
A claimant depends on an accurate, complete, and timely assessment provided by their physician(s) to substantiate their claim for disability benefits. However, often physicians do not provide sufficient information when completing the APS.
Reasons the APS may not be completed thoroughly
We conducted a study in 2020 to better understand this common problem.
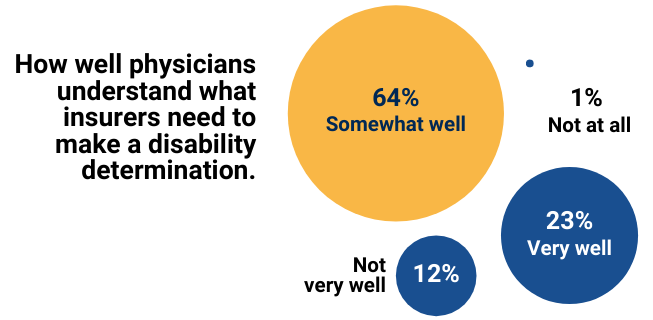
We asked a random selection of 100 physicians and health providers how well they understood what details insurers were looking for when making a disability determination. More than three-quarters of respondents acknowledged that they do not have a strong understanding of what is valuable in these forms.
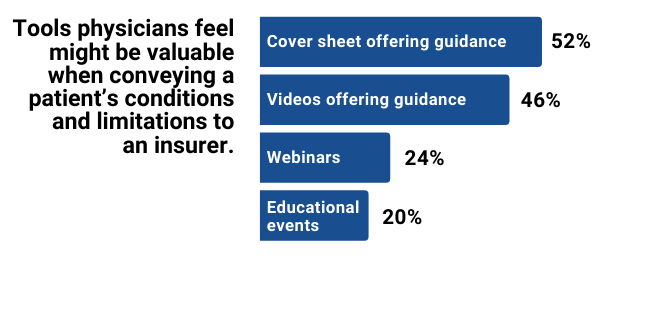
When asked about what tools or education might be valuable to them to better convey their patient’s conditions and limitations to an insurer, many said a cover sheet, video, or other multimedia content offering guidance would be helpful.
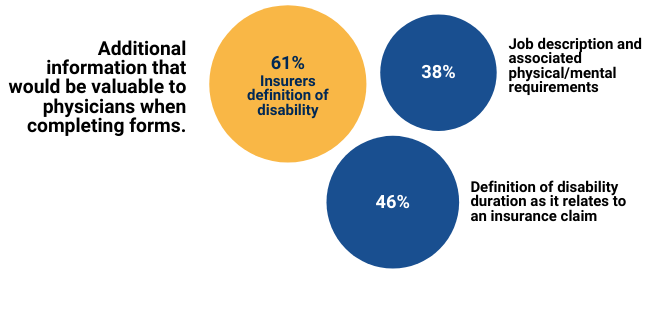
When asked if there was additional input that would be valuable, the majority of physicians felt the definition of disability would be an important piece of information to have.
While many physicians have a baseline understanding of what is required of them when completing an APS, most would value more guidance and resources from insurers.
Guidance for an attending physician
When physicians are asked to complete an APS, they should focus on compiling the following information first:
- A list of all diagnoses and any subjective symptoms or objective findings, including clinical testing and lab work.
- Dates of treatment and types of treatment (surgery, hospitalizations, medications, etc.).
- Physical limitations as it relates to the patient’s ability to do activities such as walking, standing, sitting, lifting, and more in an 8-hour work day.
A physician should also consider the following questions:
- Are there specific activities that the individual can or cannot do and what is the clinical rationale for why the individual is unable to perform certain activities?
- Are the individual’s reported symptoms consistent with clinical findings?
- Are their suggestions or comments related to the ability to return to work?
Setting expectations with attending physicians
It may be helpful for physicians to understand what happens after they complete the APS and why the form is such a crucial aspect of a disability determination.
Receiving a thoroughly completed APS lends credibility and validity to the patient’s quest for disability benefits.
The information provided on the form allows the insurer – and any medical peer reviewer – to compare the information in an attending physician’s assessment to the medical records in the patient’s file, and the patient’s self-assessment of their own capacity.
Should clarification be needed, an attending physician should be prepared to answer follow up questions in a more detailed written questionnaire, or even a phone call from a peer reviewer. The APS can serve as a starting point in this conversation and allows for a much greater understanding of the patient’s functional status.
Additionally, an attending physician should expect that they may need to complete more than one APS if their patient continues to receive care. Multiple completed forms over a range of time helps to identify improvement or regression in the patient’s condition.
Input from a physician can be vital to the expeditious and effective management of a claim, but it is also critical to keep in mind that physicians are not claim experts and may value guidance on the purpose and use of attending physician’s statements.
 This post was co-authored by one of our experienced Quality Review nurses, Bobbie Ahern, RN.
This post was co-authored by one of our experienced Quality Review nurses, Bobbie Ahern, RN.
Bobbie has worked in the disability industry for over 10 years. In her role as a Quality Review nurse at Brown & Brown, she trains physicians from various specialties how to assess information in a claimant’s disability file.