As COVID-19 began to spread rapidly across the United States in early 2020, with it came a surge of short-term disability cases inundating the absence industry. Expecting a typical year-over-year increase in the number of claims, the burst of COVID-19 claims soon took over the industry, becoming one of the top diagnosis for short-term disability claims in both 2020 and 2021. While many short-term disability claims – including those with a COVID-19 diagnosis – resolved within a matter of a month or two, a fair number of cases did not, requiring additional support and efforts to navigate “post-acute COVID-19.”
Claimants diagnosed with COVID-19 experience symptoms that can often be found in other short-term disability claims. What has separated COVID-19 claims, however, is the consistent, chronic existence of these symptoms and their impact on an individual’s ability to perform basic household and personal tasks, including engaging in work activity.
A study released by FAIR Health in June 2021 shows that more than 23 percent of people who have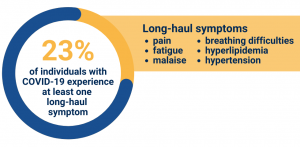 been diagnosed with COVID-19 experience at least one post-acute COVID symptom. Often the symptoms that develop post-acutely are just as debilitating, if not more, than those they developed upon initially being diagnosed with COVID-19. Among the symptoms that are most common are pain, breathing difficulties, hyperlipidemia, malaise and fatigue, and hypertension, with pain being the most consistent symptom. Individuals experiencing these ongoing symptoms are often referred to as “long-haulers” as they deal with the impacts of long-haul, or post-acute, COVID-19.
been diagnosed with COVID-19 experience at least one post-acute COVID symptom. Often the symptoms that develop post-acutely are just as debilitating, if not more, than those they developed upon initially being diagnosed with COVID-19. Among the symptoms that are most common are pain, breathing difficulties, hyperlipidemia, malaise and fatigue, and hypertension, with pain being the most consistent symptom. Individuals experiencing these ongoing symptoms are often referred to as “long-haulers” as they deal with the impacts of long-haul, or post-acute, COVID-19.
These symptoms make it difficult for individuals to return to their “pre-COVID” normal and many of them must rely on outside support, including the receipt of income replacement benefits, such as short-term disability payments. As conditions persist and prevent the return to gainful employment, the transition from short-term to long-term disability, and possibly Social Security Disability, may be inevitable.
Transitioning to long-term disability
Due to mounting medical bills or impending deadlines for health care coverage, the financial protection offered by long-term disability benefits is imperative for those dealing with post-acute COVID-19. Despite being two years into the pandemic, there is still very much unknown about COVID-19, in both its acute and post-acute phases. How long symptoms are expected to last can vary and how to identify what a long-haul symptom is seems to differ – at least slightly – among medical professionals. What we do know is how important it is that individuals transitioning to long-term disability feel supported along their journey. It is an incredibly difficult time, as many would have expected a return to normalcy once they navigated their original diagnosis. While it will not be possible or appropriate for every individual, providing options to return to work with accommodations or in another field may often be the best form of support that can be offered.
Returning to work
Returning to work after a COVID-19 diagnosis complicated by long-haul symptoms may be quite challenging for both the employee and the employer. It is important for both parties to be open about potential restrictions and what is needed to make the return-to-work both effective and productive for everyone involved. It is important to remember that this transition can be mentally, as well as physically, overwhelming, and compassion and communication will be vital in making the transition a successful one.
Additional support options for post-acute COVID complexities
-
- Social Security Disability Insurance (SSDI): SSDI benefits provide workers who expect to be out of work for at least one-year additional financial support as they navigate their health complexities. Additionally, beneficiaries who are approved benefits, and are out of work for at least twenty-nine months, qualify for Medicare health care to help offset the cost of medical expenses associated with COVID-19.
- Vocational rehabilitation: For workers who wish to return to work but need additional support, vocational rehabilitation can provide the assistance needed to successfully reenter the workforce. Any workers who are approved SSDI benefits are automatically eligible for vocational rehabilitation assistance through the Social Security Administration’s Ticket to Work program, which provides support while allowing beneficiaries to continue to receive disability income and medical coverage.
- Physical, occupational, or speech therapy: Before returning to work, those who continue to experience debilitating symptoms may need additional support in the form of therapy. Lingering physical, mental, and cognitive challenges may require additional support through therapeutic means.
Lingering impact on the absence industry
There is no doubt that the pandemic has impacted the absence industry tremendously, and the end is not yet in sight. The latest COVID-19 variant, Omicron, has proven to be the most contagious thus far, but overall, less severe than its previous counterparts. Nonetheless, people are still getting very sick and, in some instances, will need to rely on disability income replacement benefit payments. Questions then arise as reinfections occur:
-
- Is COVID-19 considered a pre-existing condition?
- Is this excluded from the policy because of the timeframe between reinfections?
- Are symptoms or conditions that develop post-acutely considered pre-existing?
It is these questions, and many more, that we expect to be answered as the industry continues to navigate COVID-19 and all its intricacies. The industry has remained flexible in the face of the unknown thus far and must continue to do so in the future. At Brown & Brown Absence Services Group, we are continuing to watch and learn as new information becomes available and will continue our commitment to releasing timing and informative industry related information as new trends and data become available. We remain ready to support our customers in navigating these complexities, together.




